megan jack, m.d.
There is a lot of interest in visual stethoscopes among our community of Deaf and hard of hearing medical professionals/students and with good reason. It allows us to have something visual to support what we are hearing if using the earpieces or to have something that allows us to auscultate without needing to hear at all. In my case, I figured my hearing wasn’t trustworthy and preferred to rely on my vision instead. I also did not want to have to fumble with taking out hearing aids, putting on bulky headphones or attaching direct audio input cables. Choosing to go with a visual stethoscope was an easy decision for me, but still presented its challenges. I have now settled with a visual stethoscope that works for me and you will get more information on that particular stethoscope in an upcoming post. For now, here are some things to keep in mind when considering a visual stethoscope (many of these points also apply to amplified stethoscopes).
Choices
While it would be great to see a new visual stethoscope come out on the market every two years as in the case with Apple products, unfortunately, the demand for visual stethoscopes is rather low. It is basically those of us involved with AMPHL who try to drive development and production forward. That means it can take years and years for a new product to finally reach the market. It is also why we have so few choices for visual stethoscopes. And due to this being a niche market, the cost of these stethoscopes are much higher than a standard stethoscope.
Technology
It has been amazing to see the technological advances over the years with cell phones, computers, printers, TVs, etc. While we do get the occasional exciting release of a new visual stethoscope, the technology is often not on par with other devices we are used to these days. For example, the old Stethographics product was only compatible with a HP pocket PC which had to be purchased from Amazon.com when the HP pocket PC was no longer being made. Likewise, the Thinklabs stethoscope app can only work with older versions of Apple products as newer models of Apple products don’t allow audio inputs of lower frequencies. The long development and production process can also mean that the technology has already begun to become outdated by the time the product reaches the market.
Battery life is something to consider as you want something that can last you at least 24 hours before needing to charge again.
But in reality, the most important thing to consider from a technological perspective is the display and use of the device. Some products show a lot of artifact that makes it difficult to interpret the display and others have a fairly clear display. Some may have one button to turn on and others might require a few more minutes for set up. Some devices have a built in display and others require a stethoscope that uses something else for a display (eg. smartphone) so this is also something to consider when choosing your stethoscope, as you may need to use both hands to hold your set up.
Backup
Depending on our career and specialties, some of us rely heavily on stethoscopes for our daily work. This means we could really struggle to do our work if our current stethoscope gets stolen, lost, damaged, or malfunctions. Our hearing counterparts can easily borrow someone else’s stethoscope, but most of us can’t. A back up is a good investment to make even though that means the cost doubles for us. I’ve had several occasions where I needed to use my second stethoscope for several weeks as my primary stethoscope had to be sent away to get fixed. The peace of mind that I have from knowing that I have a backup is so much better than the alternative of being completely stranded without one for several days when you least expect it!
Mentor(s)
Visual stethoscopes are a rarity in the medical community and thus, people usually have to figure out how to use them as they go. Most places will have no one with previous experience using visual stethoscopes but that doesn’t mean you have to figure it out alone. Ask cardiologists and respirologists if you can shadow them and have them compare what they hear to what they see on your display. They can point out what the different waveforms are based on what they hear. Ask fellow students and colleagues to let you know if any interesting patients come in so you can see different murmurs and adventitious breath sounds.
We have now covered some points to consider when choosing to go with a visual stethoscope. If you do decide to choose a visual stethoscope, have fun figuring it out! Check out the following for a basic introduction to understanding what you’re seeing on the display. Just keep in mind that these are simplified figures and what you actually see will differ depending on your display and the person/animal you are auscultating.
Basic primer on interpreting the visual display
Normal heart sounds show up as spikes to represent S1 and S2 (Figure 1). You can determine the S1 by looking for the spike that shows up just prior to the apex of the carotid pulse. S2 occurs after the pulse. If you are just eyeballing the visual display, the S1-S2 are closer together than S2-S1.
For murmurs, you have to look at the systolic phase (between S1 and S2) or the diastolic phase (between S2 and S1). If there is activity in between the spikes, you need to determine the general pattern (crescendo-descrescendo, holosystolic, or additional spike). Once you figure out which phase and the pattern, you can determine the murmur. Figure 2 is a classic example of a crescendo-descrescendo pattern that represents a systolic ejection murmur or aortic stenosis.
Figure 3 is an example of a holosystolic murmur representing mitral regurgitation.
I found the Blaufuss.org heart sound tutorial a great resource for learning auscultation of heart sounds and best of all, it is complete with phonocardiograms to illustrate the different heart sounds and murmurs! However, actual experience trumps my simplified drawings and most phonocardiogram figures that you will find. Hair, clothing, body habitus, breathing, and ambient sounds can all complicate what you are seeing on your display. The best thing you can do is to use your stethoscope as much as you can and to have people listen at the same time to verify the accuracy of your visual stethoscope. Be comfortable with different manoeuvres to help elicit murmurs and don’t be afraid to ask people to hold their breath so you can focus on heart sounds better. Just remember to tell them to breath after!
Speaking of breathing, this is how I see breath sounds with my visual stethoscope. Figure 4 shows normal inspiration and expiration, with expiration being a flat line. I have found that decreased breath sounds will have an almost flat line during the inspiration phase (watch the patient’s breathing at the same time to determine the phase). No breath sounds will be a flat line.
For crackles, I will see scattered small spikes during the expiration phase (Figure 5). I generally don’t see crackles during inspiration due to the air entry sounds, but if the breath sounds are coarse, I can see larger spikes in both phases. A tip to distinguish between fine and coarse crackles: get the patient to cough. If the crackles disappear, then those were fine crackles.
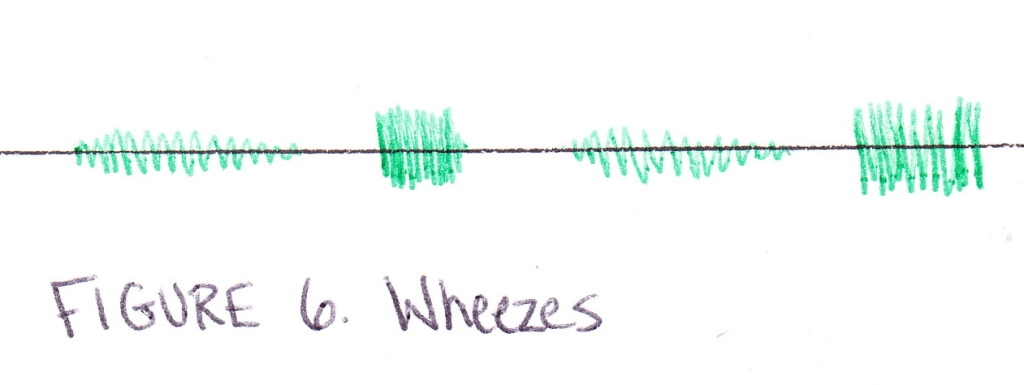
Wheezes are like a dense holosystolic murmur often during expiration (Figure 6).
However, depending on which visual display you use, the breath sounds may display differently than my diagrams. Easyauscultation.com and PracticalClinicalSkills.com has examples of waveforms for different breath sounds that you can check out and you will notice that how I’ve shown the breath sounds are different than the waveforms shown on these websites.
For bowel sounds, I basically make note of whether sounds are present or not. No bowel sounds will show up as a flat line. Bowel sounds should show up as various spikes. As with a normal stethoscope, you should be patient and watch for some time to ensure there are bowel sounds.
We here at AMPHL know stethoscopes are one of the bigger challenges most of us have to figure out and it can be discouraging not to have the perfect stethoscope out there. Believe me, I am still looking! But even though you may have to try out a few stethoscopes before settling on one that works the best for you, you still have everything you need to become a great clinician. The history and your comprehensive physical exam will help guide your diagnosis and management far more than just a stethoscope will.
ABOUT THE AUTHOR
Megan Jack, M.D. is a family medicine physician practicing in Winnipeg, Canada. She received her medical degree from the University of Manitoba in 2013, becoming the first deaf Canadian to do so. Megan served on the AMPHL Board between 2013 and 2017 and was Secretary from 2015 to 2017.
SUGGESTED CITATION
Jack, M. (2014). Seeing the Sounds: How to Use Visual Stethoscopes. Association of Medical Professions with Hearing Losses.